RPM and Diabetes Disease
Presently, diabetes has no cure. But it can be managed.
Diabetes occurs when you have high blood glucose. And while symptoms may be more or less severe, the disease is always equally serious and requires active monitoring.
In the past decade, over 9% percent of the U.S. population had diabetes—including 1 in 4 people over 65 years old. And over a quarter of them didn’t know they had the disease. Complications from diabetes can include heart disease, kidney disease, stroke, vision problems, nerve damage, and more.
There are two main types of diabetes:
Type 1
Type 1 diabetes means that you need to take insulin every day in order to maintain balanced blood sugar. That’s because your body both: does not make its own insulin, and attacks the cells in your pancreas that would otherwise attempt to create insulin. Type 1 is often diagnosed in young people (although it can manifest at any age) and should be treated urgently, as lack of insulin intake is fatal.
Type 2
Type 2 diabetes can be diagnosed at any age, but it often presents in middle aged and older individuals. It can develop if you have a family history of diabetes or if you are overweight. Certain medical conditions (such as high blood pressure) and even certain factors like race might increase your chance of developing it. For these reasons, it is the more common of the two types of diabetes. Rather than attacking the cells that make insulin, your body simply does not make or use insulin as well as it should.
However, there are a few other types of diabetes. For example, gestational diabetes can occur in pregnant women—yet, it almost always resolves upon giving birth. Those who experience it are more likely to have type 2 diabetes later in life. Other types (which are far rarer) are monogenic diabetes and cystic fibrosis-related diabetes.

What Is Insulin?
Where do you get all the energy to move, work, accomplish tasks, and get through the day? Your body uses glucose (blood sugar)—which comes from food—to create the energy that powers you. But first, insulin has to help the glucose enter the cells in your muscle, liver, and fat, where it’s converted into energy.
The pancreas is responsible for making insulin and releasing it into your blood. This typically happens right after you eat (and ingest glucose) so that you’re primed to convert that energy. As it’s successfully converted, the glucose is reduced back to a normal, sustainable range within your blood.
Therefore, you both have the energy you need, and do not have blood sugar you don’t need, all because of insulin.
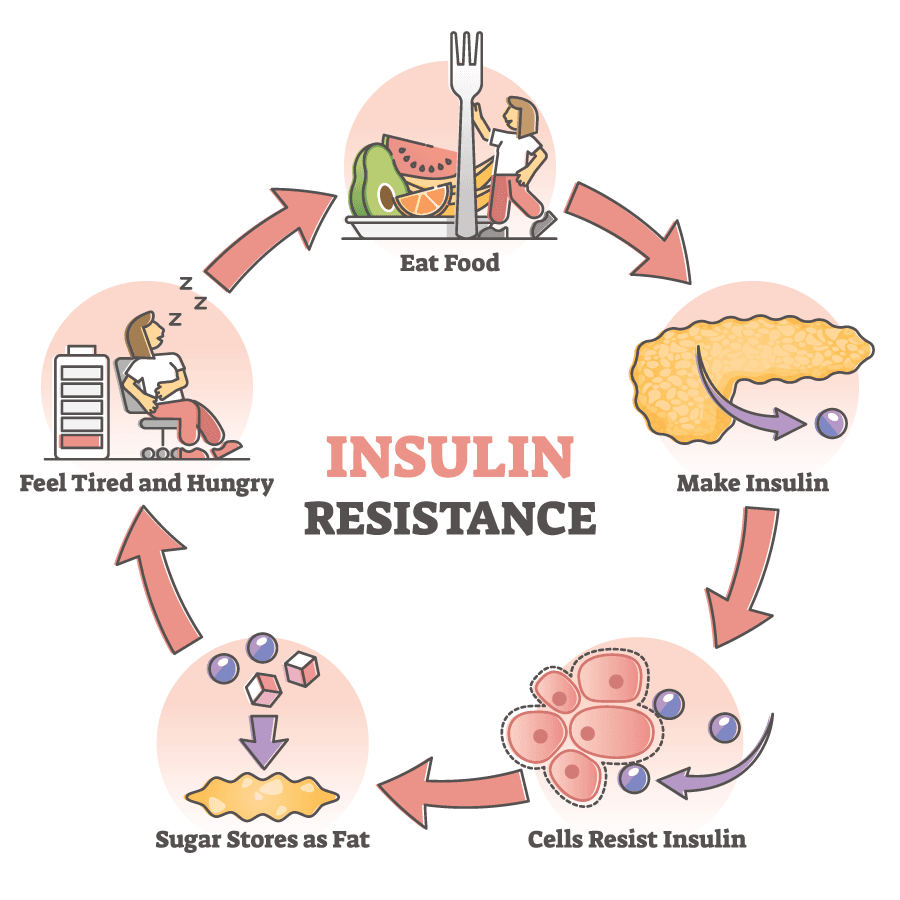
What Is Insulin Resistance?
If your cells are not reacting appropriately to insulin, and therefore not absorbing glucose, then your pancreas will assume you just need more insulin to help get that glucose level back in range. Sometimes, this is successful, and your body will naturally adapt to what is otherwise known as insulin resistance. But it can also lead to glucose spikes and prediabetes.
What Is Prediabetes?
When you have above-average glucose levels in your blood (and your cells are not absorbing it, or your pancreas is not creating insulin quite fast enough to stabilize your body fast enough), then you might have prediabetes. In this case, your levels would not be quite high enough to qualify as diabetes.
Typically, this occurs in individuals with insulin resistance, but it might also be because the beta cells in the pancreas are not in fact making insulin fast enough (regardless of the body’s ability to absorb glucose and respond to that insulin well enough). If you consistently or continuously fail to create enough insulin and manage your blood sugar, you could develop type 2 diabetes, so it is important to monitor this condition. Over 84 million adults (or 1 in 3) are prediabetic in the U.S.
What Are Risk Factors for Insulin Resistance or Prediabetes?
Risk factors for insulin resistance and prediabetes include:
- age
- obesity
- a parent, brother, or sister with diabetes
- race (African-American, AAPI, Hispanic/Latino, Native American)
- physical inactivity
- health conditions (high blood pressure, metabolic syndrome)
- a history of gestational diabetes
- a history of heart disease or stroke
- polycystic ovary syndrome (PCOS)
You might be unable to change your age, family history, and ethnicity, but you do have control over lifestyle habits like healthy eating and pursuing physical activity. These choices can lower your chances of developing insulin resistance or prediabetes.
Experts believe that a primary cause of insulin resistance is obesity. This is especially true is someone is carrying too much fat in the abdomen and around the organs (which is known as visceral fat). This may lead to chronic inflammation in the body and play a role in the development of type 2 diabetes, cardiovascular disease, or fatty liver disease. Regular physical activity, on the other hand, can cause long-lasting changes in the body that reduces the risk of insulin resistance and prediabetes.
How Do You Diagnose Insulin Resistance and Prediabetes?
There are few obvious symptoms of prediabetes, so it’s important to get a diagnosis from a doctor. However, doctors do not usually test for insulin resistance and there are not typically symptoms. The most accurate test for insulin resistance is complicated and used mostly for research.
One symptom of prediabetes is acanthosis nigricans, which shows itself as darkened skin in the armpit or on the neck (back and sides). Skin tags can accompany the discoloration. In rare cases, prediabetes can lead to retinopathy; however, this is more likely to occur in those with diabetes.
For a formal diagnosis, you will likely undergo a fasting plasma glucose (FPG) test or A1C. Less often, doctors use the oral glucose tolerance test (OGTT), which is more expensive and not as easy to give. The OGTT demonstrates how your body processes glucose immediately after a meal and can be a very accurate test, but it is most often used to determine gestational diabetes. The FPG also reflects glucose levels accurately as of the time of the test, but it can be less popular for pregnant women because it requires fasting. Meanwhile, the A1C observes levels over the past three months (which is not always useful for determining an acute and temporary condition). The A1C is a common choice otherwise, although it is not as sensitive with its results as, for example, the OGTT.
Here are what the results would reflect for prediabetes with each test:
- A1C—5.7 to 6.4 percent
- FPG—100 to 125 mg/dL (milligrams per deciliter)
- OGTT—140 to 199 mg/dL
How Do You Treat Prediabetes?
You have up to a 50% chance of developing diabetes in the next decade if you’re already prediabetic. Therefore, regular at-home monitoring will be an important part of your preventive and proactive care.
This will include using an at-home blood glucose meter or similar device. The frequency of your testing will be determined by your physician.
Your self-monitoring device reports your blood sugar levels in milligrams of sugar per deciliter (mg/dL) or millimoles of sugar per liter (mmol/L). Your results reflect your glucose measurement at the exact time of the test; therefore, it is likely to change throughout the day based on when and what you eat, as well as exercise and other variables. Because of this, your monitor can serve a dual purpose of informing your lifestyle habits and tracking your outcomes toward your intended blood sugar and health goals.
For example, if your A1C target is below 7%, your self-monitoring blood sugar levels should be, on average, below 154 mg/dL (8.6 mmol/L).
How Do You Treat Prediabetes?
You have up to a 50% chance of developing diabetes in the next decade if you’re already prediabetic. Therefore, regular at-home monitoring will be an important part of your preventive and proactive care.
This will include using an at-home blood glucose meter or similar device. The frequency of your testing will be determined by your physician.
Your self-monitoring device reports your blood sugar levels in milligrams of sugar per deciliter (mg/dL) or millimoles of sugar per liter (mmol/L). Your results reflect your glucose measurement at the exact time of the test; therefore, it is likely to change throughout the day based on when and what you eat, as well as exercise and other variables. Because of this, your monitor can serve a dual purpose of informing your lifestyle habits and tracking your outcomes toward your intended blood sugar and health goals.
For example, if your A1C target is below 7%, your self-monitoring blood sugar levels should be, on average, below 154 mg/dL (8.6 mmol/L).
Refer to the following chart:
A1C level | Estimated average blood sugar level |
|---|---|
6% | 126 mg/dL (7 mmol/L) |
7% | 154 mg/dL (8.6 mmol/L) |
8% | 183 mg/dL (10.2 mmol/L) |
9% | 212 mg/dL (11.8 mmol/L) |
10% | 240 mg/dL (13.4 mmol/L) |
11% | 269 mg/dL (14.9 mmol/L) |
12% | 298 mg/dL (16.5 mmol/L) |
What Are the Benefits of Remote Patient Monitoring?
Today, Remote Patient Monitoring (RPM) allows physicians to ensure your diabetes is being managed promptly and accurately. You benefit from the most sophisticated technology for timely insights and coordinated care.
With RPM, you can measure, upload, and wirelessly transmit your blood pressure and glucose readings to your health care team.
Wearable devices make it effortless and automatic to record and share information. As part of your holistic health care approach, you can also track heart rate, gait, tremors, physical activity, and sleep patterns. Home monitoring devices can also help older people by detecting abnormal activities (for example, detecting falls and alerting your physician or an emergency care provider).

